By Dr. Matthias Wiederholz with Performance Pain and Sports Medicine
Quadruple Board-Certified in Physical Medicine & Rehabilitation, Sports Medicine, Pain Medicine, and Regenerative Medicine
Updated January 22, 2026
Medically reviewed and updated for accuracy
Quick Insights
An annular fissure is a tear in the tough outer layer of a spinal disc, known as the annulus fibrosus. These tears can cause localized back pain, radiating discomfort into the legs, and reduced mobility. Annular fissures develop from age-related disc degeneration, repetitive strain, trauma, or poor posture. MRI imaging often reveals a high-intensity zone (HIZ) at the site of the tear. Most annular fissures respond well to conservative treatment when addressed early, while persistent cases may benefit from minimally invasive procedures like the Discseel® Procedure.
Key Takeaways
- An annular fissure and an annular tear refer to the same condition—a split in the disc’s outer annulus fibrosus layer.
- Types include radial, concentric, and peripheral tears; location classifications include posterior, central, and foraminal annular fissures.
- Symptoms range from localized back pain to radiating leg pain, numbness, and weakness when nerves become irritated.
- MRI high-intensity zone (HIZ) findings correlate with annular disruption but require clinical context for accurate diagnosis.
- Treatment progresses from conservative care to minimally invasive options like epidural injections or the Discseel® Procedure for persistent symptoms.
Why It Matters
Living with an annular fissure can make everyday activities—sitting at your desk, driving across Houston, or playing with your children—miserable. Left untreated, disc tears may progress to disc herniation or chronic discogenic pain. Recognizing annular fissure symptoms early empowers you to seek effective care, improve your quality of life, and return to the activities you love without constant pain.
What Is an Annular Fissure?
As an interventional pain specialist, I evaluate patients daily who are struggling with back pain caused by spinal disc damage. An annular fissure is one of the most common yet frequently misunderstood conditions I treat.
An annular fissure is a tear in the annulus fibrosus—the tough, fibrous outer ring that surrounds and contains the soft gel-like center of your spinal disc. Think of your disc like a jelly donut: the annulus fibrosus is the outer dough, and the nucleus pulposus is the jelly inside. When the outer layer develops a crack or tear, it creates a pathway for inflammatory chemicals to leak out and irritate nearby nerves.
According to clinical reference literature from the National Library of Medicine, annular fissures can occur with or without disc protrusion and represent a spectrum of disc pathology ranging from minor tears that heal naturally to significant defects that cause chronic pain.
The terms “annular fissure” and “annular tear” are used interchangeably in medical literature. Whether your MRI report says “annular fissure,” “annular tear,” or “annular disruption,” these all describe the same underlying condition—a split in your disc’s protective outer layer.
Types of Annular Fissures
Annular fissures are classified by both their structural pattern and their location within the disc. Understanding these distinctions helps guide treatment decisions and predict outcomes.
Structural Classification
Radial tears extend from the inner nucleus pulposus outward through the annulus fibrosus layers. These tears follow the path of least resistance and are most commonly associated with disc degeneration. Radial tears can allow nuclear material to migrate outward, potentially leading to disc herniation.
Concentric tears run parallel to the disc’s outer edge, separating the lamellae (layers) of the annulus without extending inward toward the nucleus. These tears result from shearing forces and are often associated with rotational injuries or repetitive twisting movements.
Peripheral tears occur at the outer edge of the annulus where it attaches to the vertebral body. These tears may develop from trauma or degenerative changes at the disc-bone junction and can be particularly painful due to the rich nerve supply in this region.
Location Classification
Posterior annular fissure: Located at the back of the disc, closest to the spinal canal and nerve roots. Posterior tears are the most clinically significant because they can directly irritate the spinal nerves, causing radiating leg pain. Research examining enhancing annular fissures and high-intensity zones demonstrates that posterior tears correlate strongly with pain responses during diagnostic testing.
Central annular fissure: Located in the middle portion of the posterior disc. Central tears can cause axial back pain and may progress to central disc protrusion if left untreated.
Foraminal annular fissure: Located near the neural foramen—the opening where spinal nerves exit the spine. Foraminal tears can compress exiting nerve roots, causing specific dermatomal pain patterns down the leg.
Dorsal annular fissure: Another term for posterior-located tears, “dorsal” simply means “toward the back.” Dorsal annular fissures carry the same clinical implications as posterior tears.

Causes and Risk Factors
Annular fissures develop when the disc’s outer layer weakens or sustains damage. In my Houston practice, I’ve identified several consistent patterns among patients who develop these tears.
Primary Causes
Age-related disc degeneration: As you age, your discs naturally lose water content and elasticity. The annulus fibrosus becomes less flexible and more prone to cracking. This degenerative process affects most adults by middle age, though not everyone develops symptomatic tears.
Repetitive stress: Occupations requiring frequent bending, lifting, or twisting place ongoing strain on spinal discs. Workers in construction, healthcare, and warehouse industries face elevated risk. Even desk workers who maintain poor posture for hours daily can develop annular tears from sustained compressive loading.
Acute trauma: Falls, motor vehicle accidents, and sports injuries can cause sudden disc damage. A single high-force event can tear an otherwise healthy annulus, particularly in younger patients.
Disc bulge with annular fissure: These conditions frequently coexist. When the annulus weakens, the disc may bulge outward while simultaneously developing tears. Imaging studies demonstrate that annular fissures often accompany other structural changes including vertebral endplate damage and disc height loss.
Risk Factors
Several factors increase your likelihood of developing annular fissures:
- Smoking—nicotine reduces blood flow to discs, impairing healing capacity
- Obesity—excess weight increases compressive loads on lumbar discs
- Sedentary lifestyle—weak core muscles provide inadequate spinal support
- Genetic predisposition—family history of disc disease increases risk
- Previous spine injury—prior trauma weakens disc structure
The lumbar spine bears the greatest mechanical load, making annular fissure lumbar spine locations most common. The L4-L5 and L5-S1 levels are particularly vulnerable due to their position at the base of the mobile spine. For detailed information about L5-S1 pathology, see our comprehensive guide to L5-S1 pain causes, symptoms, and treatment.
Annular Fissure Symptoms
Annular fissure symptoms vary widely depending on the tear’s location, size, and whether it irritates nearby nerves. Some patients have annular tears discovered incidentally on MRI without any symptoms, while others experience debilitating pain.
Common Symptoms
Localized back pain: Sharp, aching, or burning pain at the site of the fissure represents the most frequent complaint. This discogenic pain originates from the tear itself, as the outer annulus contains pain-sensing nerve fibers. Pain typically worsens with sitting, bending forward, or lifting.
Radiating pain: When inflammatory chemicals from the torn disc irritate spinal nerve roots, pain can radiate into the buttocks, hips, or legs. A posterior annular fissure or central annular tear is most likely to cause these radiating symptoms.
Muscle spasm: Your body’s protective response to disc injury often includes paraspinal muscle tightness. These spasms can cause additional stiffness and discomfort.
Reduced range of motion: Stiffness and difficulty bending, twisting, or straightening your back commonly accompany annular tears.
Pain with specific movements: Symptoms frequently worsen with activities that increase intradiscal pressure—sitting, coughing, sneezing, or bearing down.
When Nerve Involvement Occurs
If an annular fissure allows disc material to contact or compress a spinal nerve, additional symptoms may develop:
- Numbness or tingling in the leg or foot
- Weakness in specific muscle groups
- Sharp, shooting pain following a dermatomal pattern
- Difficulty walking or maintaining balance
These neurological symptoms require prompt evaluation. For more information about nerve-related symptoms, explore our article on herniated disc symptoms, causes, and treatment.
When to Seek Immediate Medical Attention
Certain symptoms indicate potential serious nerve involvement requiring urgent evaluation:
- Loss of bladder or bowel control
- Progressive leg weakness or numbness
- Sudden inability to walk
- Numbness in the groin or inner thighs (saddle anesthesia)
These signs may indicate cauda equina syndrome—a medical emergency. If you experience any of these symptoms, seek immediate care.
Diagnosis of Annular Fissures
Accurate diagnosis requires combining your clinical history, physical examination findings, and imaging studies. In my practice, I use a systematic approach to identify annular fissures and determine their clinical significance.
Clinical Evaluation
The diagnostic process begins with a thorough history. I ask about pain location, duration, aggravating factors, and any neurological symptoms. Physical examination includes assessing range of motion, nerve function, and reproducing pain with specific maneuvers.
Imaging Studies
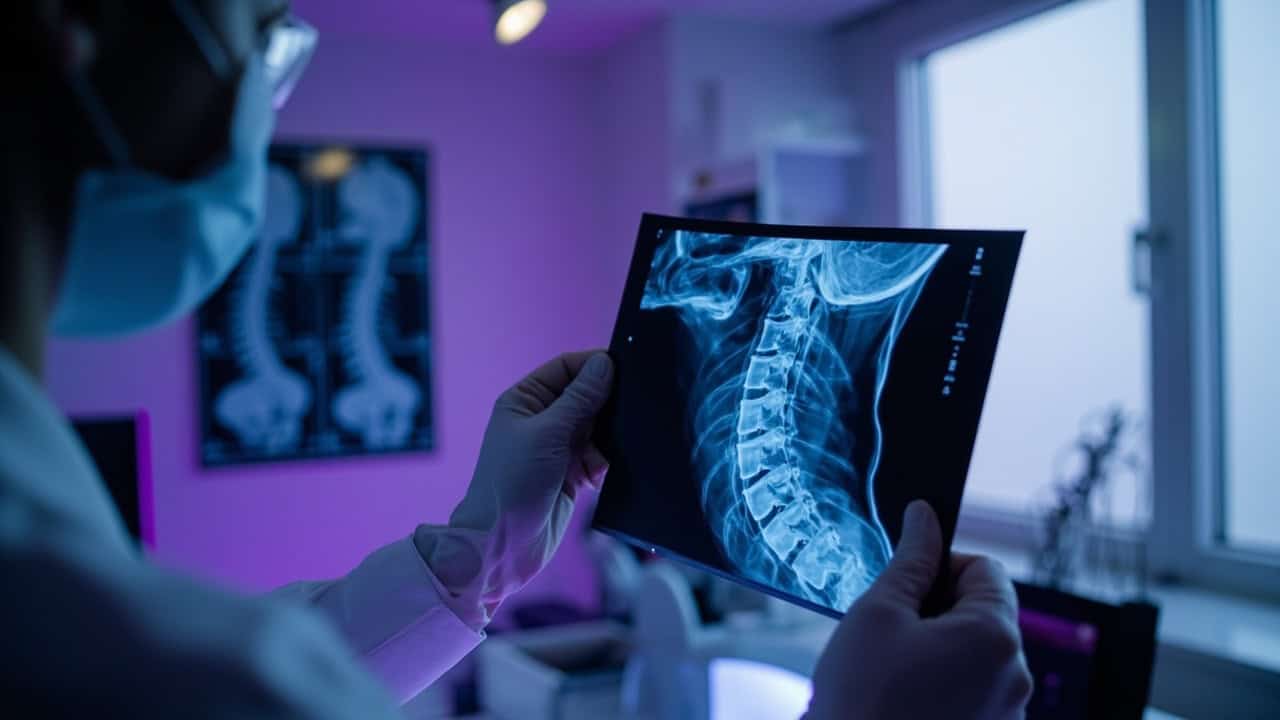
MRI (Magnetic Resonance Imaging): MRI is the primary imaging modality for detecting annular fissures. A characteristic finding is the high-intensity zone (HIZ)—a bright signal on T2-weighted images indicating fluid within the annular tear. Research correlating MRI with discography confirms that HIZ findings reflect annular disruption, though clinical context remains essential for interpretation.
CT scan: While less sensitive than MRI for soft tissue, CT provides excellent bone detail and may reveal associated vertebral changes or calcification.
Discography: In select cases where diagnosis remains uncertain, provocation discography can confirm whether a specific disc is your pain generator. This test involves injecting contrast into the disc and assessing your pain response. Studies examining enhancing annular fissures with provocation discography demonstrate that this technique enhances diagnostic accuracy when imaging findings require clinical correlation.
Important Diagnostic Considerations
Not every annular fissure visible on MRI causes pain. Imaging studies of asymptomatic individuals frequently reveal disc abnormalities. The key is correlating imaging findings with your specific symptoms and examination findings to confirm the disc as your true pain source.
Treatment Options for Annular Fissures
Treatment for annular fissures follows a stepwise approach, beginning with conservative measures and progressing to interventional options when symptoms persist. North American Spine Society guidelines recommend evidence-based pathways that match treatment intensity to symptom severity.

Conservative Treatment
Most annular fissures respond well to conservative management, particularly when addressed early:
Activity modification: Avoiding positions and movements that increase disc pressure—prolonged sitting, heavy lifting, forward bending—reduces stress on the damaged annulus.
Physical therapy: A targeted exercise program strengthens core muscles, improves spinal stability, and promotes proper movement patterns. Therapy should progress gradually to avoid aggravating the tear.
Medications: NSAIDs reduce inflammation and pain. Muscle relaxants may help if spasm is significant. Short-term use is generally recommended to avoid long-term side effects.
Heat and cold therapy: Alternating applications can reduce muscle spasm and temporarily relieve pain.
Lifestyle modifications: Weight management, smoking cessation, and ergonomic improvements support disc health and healing.
Minimally Invasive Procedures
When conservative care fails to provide adequate relief, minimally invasive procedures offer targeted treatment without the risks of open surgery:
Epidural steroid injections: Delivering anti-inflammatory medication directly to the affected area can reduce nerve root irritation and provide meaningful pain relief. This procedure serves both diagnostic and therapeutic purposes.
Intradiscal procedures: Several interventional techniques target the disc itself. Systematic reviews examining regenerative approaches including thermal annular procedures demonstrate clinically meaningful pain relief for appropriately selected patients.
The Discseel® Procedure: This innovative treatment uses a biologic fibrin sealant injected directly into the damaged disc. The sealant seals annular tears and stimulates natural collagen formation, promoting disc healing from within. As one of only three Master Instructors worldwide—trained directly by the procedure’s inventor—I’ve performed hundreds of Discseel® procedures at our Houston Discseel® center.
The Discseel® Procedure represents a mechanism-based approach: rather than masking symptoms, it addresses the underlying annular damage that generates pain.
Ready to find out if you’re a candidate? See if you qualify for the Discseel® Procedure by completing our brief screening form.
Surgical Options
Surgery is reserved for severe cases—typically when minimally invasive treatments have failed or when neurological compromise requires urgent intervention:
Microdiscectomy: Removes herniated disc material pressing on nerves. This procedure addresses the herniation but does not repair the underlying annular tear.
Spinal fusion: Joins two or more vertebrae to eliminate motion at the painful segment. Fusion carries higher risks and longer recovery than minimally invasive options and should be considered only after exhausting other approaches.
I recommend surgical intervention only when absolutely necessary, as outcomes vary and complications are possible.
Living with an Annular Fissure
Many patients manage annular fissures successfully with appropriate treatment and lifestyle modifications. Understanding your condition empowers you to make informed decisions about daily activities and long-term care.
Activity Recommendations
Low-impact activities like walking, swimming, and cycling typically cause less disc stress than high-impact sports. Core strengthening exercises support spinal stability. Proper lifting technique—bending at the knees rather than the waist—protects damaged discs from additional strain.
Long-Term Outlook
Small annular fissures may heal naturally over time with appropriate conservative care. Larger tears or those causing persistent symptoms often benefit from interventional treatment. The key is matching treatment intensity to your specific situation and goals.

Annular Fissure Treatment in Houston
Houston’s active community faces unique challenges when it comes to spine health. The city’s demanding work environments and year-round outdoor activities can stress spinal discs.
As the first physician to bring the Discseel® Procedure to Houston, I’ve treated patients from throughout the greater Houston area—from the Medical Center to Katy, Sugar Land to The Woodlands. Our Houston location provides comprehensive evaluation and treatment for annular fissures and other disc conditions.
Whether you’re dealing with a small annular fissure causing intermittent symptoms or a disc protrusion with annular fissure requiring advanced intervention, our team develops individualized treatment plans based on your specific pathology, symptoms, and goals.
Conclusion
An annular fissure is a tear in your spinal disc’s outer layer that can cause persistent back pain, radiating symptoms, and reduced quality of life. Understanding the types—radial, concentric, and peripheral tears at posterior, central, or foraminal locations—helps guide appropriate treatment.
Most patients respond well to conservative care, including physical therapy, activity modification, and anti-inflammatory medications. When symptoms persist despite appropriate conservative management, minimally invasive options like epidural injections and the Discseel® Procedure offer targeted treatment that addresses the underlying annular damage.
If you’re experiencing back pain from an annular fissure, early evaluation and treatment can prevent progression and help you return to the activities you value. Contact our team to schedule a consultation and discuss your treatment options.
For those interested in learning whether they may be candidates for the Discseel® Procedure, complete our brief screening form to take the first step toward lasting relief.
This article is for educational purposes only and should not be used as a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition or treatment options. Never disregard professional medical advice or delay in seeking it because of something you have read in this article.
Frequently Asked Questions
What is the difference between an annular fissure and an annular tear?
An annular fissure and an annular tear are the same condition—both terms describe a split or crack in the annulus fibrosus, the outer layer of your spinal disc. Medical literature and imaging reports use these terms interchangeably. Whether your MRI says “annular fissure,” “annular tear,” or “annular disruption,” the underlying pathology is identical.
Can an annular fissure heal on its own?
Small annular fissures may heal naturally over time with appropriate conservative care—rest, physical therapy, and activity modification. However, larger tears or those in areas with poor blood supply often do not heal completely on their own. Persistent symptoms after several months of conservative treatment may indicate the need for interventional options that promote disc healing, such as the Discseel® Procedure.
What does a posterior annular fissure mean on my MRI?
A posterior annular fissure means you have a tear at the back of your disc, closest to the spinal canal and nerve roots. This location is clinically significant because posterior tears can directly irritate spinal nerves, causing radiating leg pain in addition to back pain. Posterior annular fissures often benefit from targeted treatment due to their proximity to neural structures.
Is disc bulge with annular fissure serious?
A disc bulge with annular fissure represents combined pathology that may cause more symptoms than either condition alone. The bulging disc can compress nerves while the tear releases inflammatory chemicals that irritate surrounding tissues. Treatment depends on your specific symptoms—many patients respond to conservative care, while others may need interventional procedures to address both the bulge and the tear.
How long does recovery take after Discseel® for an annular fissure?
Most patients return to light activities within days of the Discseel® Procedure. However, the biologic healing process takes time—the fibrin sealant stimulates collagen formation and tissue regeneration over weeks to months. Most patients notice progressive improvement over 3-6 months as the disc heals. Full benefit may take up to a year as the repaired annulus regains structural integrity.
What causes annular fissure at L5-S1 specifically?
The L5-S1 level bears tremendous mechanical load as the junction between the mobile lumbar spine and the fixed sacrum. This transitional zone experiences high compressive and shear forces with daily activities. Combined with age-related degeneration, these mechanical stresses make annular fissure L5-S1 the most common location for disc tears. For comprehensive information about this spinal level, see our guide to L5-S1 pain and treatment.