By Matthias Wiederholz, MD
Quadruple Board-Certified in Physical Medicine & Rehabilitation, Sports Medicine, Pain Medicine, and Regenerative Medicine
Quick Insights
Recovery from back surgery varies widely based on procedure type and individual factors. Microdiscectomy patients often resume light activities within 2-6 weeks, while spinal fusion may require 3-6 months for basic function and up to a year for full recovery. However, research shows not all patients achieve complete healing. Registry data from cervical myelopathy surgery shows that approximately 65% of working patients return to work within one year, rising to 75% by three years. The reasons for not returning to work among the remaining patients are varied and may include ongoing limitations, personal choice, or other factors. For Lawrenceville residents considering back surgery, understanding these realistic timelines and outcomes helps set appropriate expectations. Recovery depends on surgical timing, overall health, and whether the procedure addresses underlying disc pathology.
Key Takeaways
- Longer preoperative symptom duration correlates with worse postsurgical outcomes, particularly after six months of conservative care failure.
- Adjacent segment degeneration and persistent disc pathology can cause ongoing pain even after technically successful decompression procedures.
- Structured rehabilitation with early mobilization significantly improves functional recovery and reduces complication risk after spine surgery.
- Patient selection and surgical timing determine outcomes more than the specific surgical technique used for cervical radiculopathy.
Why It Matters
Understanding realistic recovery expectations helps you make informed decisions about spine surgery and recognize when persistent symptoms signal unresolved disc pathology rather than normal healing. Many patients continue experiencing limitations because surgery addressed nerve compression but not underlying disc degeneration. Knowing these factors empowers you to seek comprehensive evaluation when recovery stalls, potentially avoiding years of unnecessary restriction and exploring mechanism-based alternatives that target root causes.
Introduction
As a quadruple board-certified physician specializing in spine care, I’ve guided countless Lawrenceville residents through the recovery process after back surgery. Understanding how long to recover from back surgery is one of the most common questions I hear, and the answer isn’t simple. Recovery timelines vary dramatically based on procedure type, individual health factors, and whether the surgery addresses the underlying disc pathology causing your pain. For those seeking specialized care, my expertise as a physician in advanced spine treatments ensures a comprehensive approach for every patient.
Consensus guidelines on return-to-work timelines show that microdiscectomy patients often resume light activities within 2-6 weeks, while spinal fusion may require 3-6 months for basic function and up to a year for full recovery. However, research reveals a more complex reality: not all patients achieve complete healing. A nationwide registry study of cervical myelopathy surgery found that approximately 65% of working patients had returned to work at one year, increasing to 75% by three years. The reasons for not returning to work among the remaining patients are varied and may include ongoing limitations, personal choice, or other factors.
The critical factor many patients in Lawrenceville and surrounding areas like Ewing and Hopewell don’t understand is that surgical success depends on timing, overall health, and whether the procedure truly addresses the structural disc damage generating your pain. When surgery focuses only on decompressing nerves without repairing annular tears or disc degeneration, persistent symptoms often continue despite technically successful operations.
As you weigh your options or struggle with ongoing symptoms after surgery, it’s also important to understand back pain management strategies and alternatives that target the root cause of your discomfort.

What Is the Typical Recovery Timeline After Back Surgery in Lawrenceville?
Recovery timelines vary significantly based on the specific procedure you undergo. Consensus guidelines on return-to-work expectations provide evidence-based ranges that help set realistic expectations. For microdiscectomy, most patients resume light activities within two to six weeks. Full recovery typically occurs between three and six months. Lumbar fusion requires substantially more time—three to six months for basic function and six to twelve months for complete healing.
Anterior cervical discectomy and fusion follows a similar staged progression. Patients often return to desk work within four to six weeks. Physical jobs may require three to six months before full duty resumes. I emphasize to patients in my Lawrenceville practice that these timelines represent averages, not guarantees. Your individual recovery depends on multiple factors beyond the surgery itself.
For a deeper understanding of other surgical approaches, learn about L5-S1 herniated disc surgery and targeted treatments.
The concept of “recovery” also varies by activity type. Driving typically resumes within two to four weeks for most procedures. Light-duty work may begin at four to six weeks. Heavy labor or contact sports often require six months or longer. Understanding these distinctions helps you plan realistically for how long to recover from back surgery based on your specific lifestyle demands.

Factors That Influence How Long Recovery Takes
Several key factors determine your recovery trajectory after spine surgery. Age and overall health status significantly impact healing capacity. Younger patients with fewer comorbidities typically recover faster than older individuals with diabetes, cardiovascular disease, or obesity. Smoking dramatically slows bone fusion and soft tissue healing, often extending recovery by months.
The timing of your surgery matters more than many patients realize. Research demonstrates that longer preoperative symptom duration correlates with worse postsurgical outcomes. When patients wait beyond six months with persistent symptoms, nerve damage and muscle deconditioning become more difficult to reverse. I often see patients who delayed surgery for years, then wonder why recovery takes longer than expected.
Your occupation and physical demands directly influence return-to-work timelines. Desk workers may resume modified duty within weeks. Construction workers or nurses performing patient transfers may need several months. Structured rehabilitation protocols and early mobilization strategies optimize recovery regardless of job type. Patients who actively participate in physical therapy, follow activity restrictions, and gradually progress their exercises consistently achieve better outcomes than those who remain sedentary or push too aggressively too soon.
Psychological factors also play a substantial role. Fear of reinjury, depression, and catastrophic thinking about pain can delay functional recovery even when surgical decompression was technically successful. I address these concerns directly with patients because mental preparation influences physical healing.
Interested in recovery after a different spinal level? See our resource on L5-S1 pain causes, symptoms, and treatment.

Do Patients Ever Fully Recover From Back Surgery?
The honest answer is that not all patients achieve complete recovery. A nationwide registry study found that approximately 65% of working patients with cervical myelopathy had returned to work within one year of surgery, increasing to 75% by three years. The reasons for not returning to work among the remaining patients are varied and may include ongoing limitations, personal choice, or other factors. These statistics reflect real-world outcomes across diverse patient populations and surgical indications.
Clinical improvement doesn’t always translate to full functional restoration. Some patients experience substantial pain reduction and improved mobility yet cannot return to their previous occupation or activity level. Others achieve excellent symptom relief but develop new limitations from adjacent segment degeneration or altered spinal biomechanics after fusion.
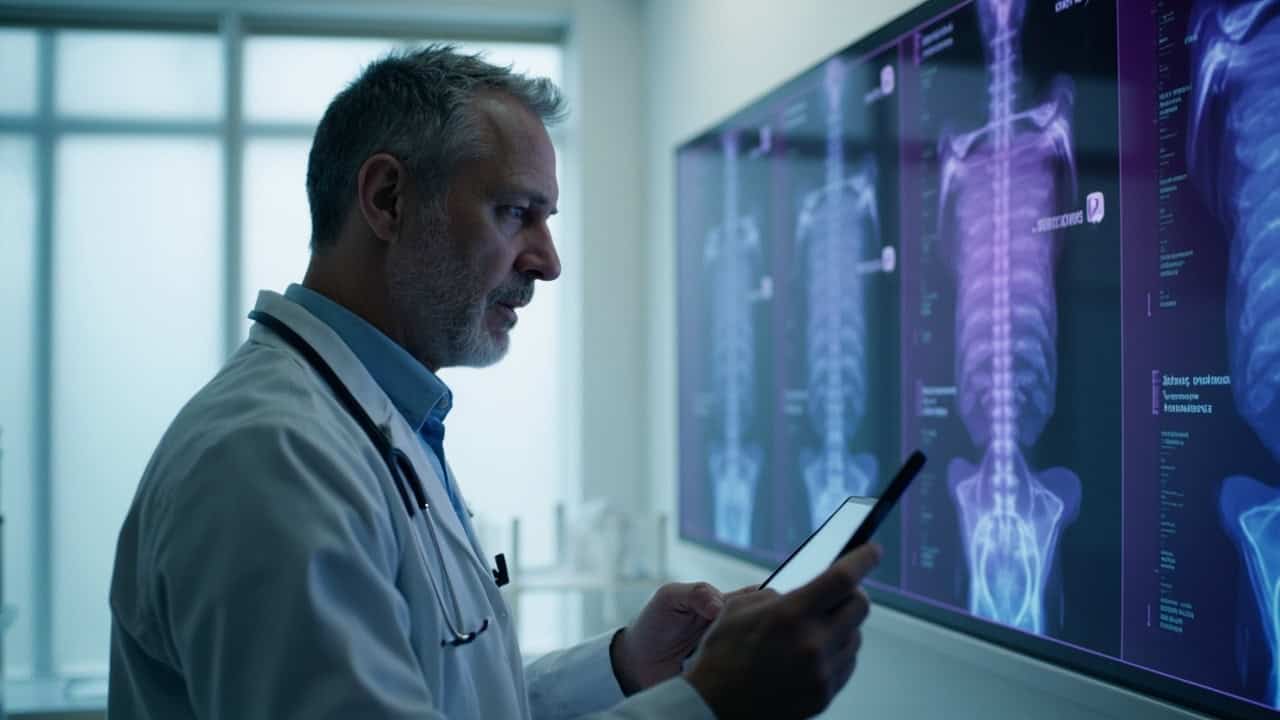
Studies on cervical decompression surgery show meaningful improvements in function and quality of life for many patients with myelopathy. However, the degree of improvement varies widely. Patients with severe, long-standing compression may experience partial recovery rather than complete symptom resolution. Nerve damage that occurred before surgery may be permanent.
To explore the question, do you ever fully recover from back surgery? It’s important to take a realistic approach, as discussed here and in our guides about herniated disc recovery.
In my practice, I observe three general recovery patterns. Some patients achieve excellent outcomes with minimal residual symptoms. Others experience significant improvement but retain some functional limitations. A smaller group continues struggling with persistent pain despite technically successful surgery. Understanding these possibilities helps you make informed decisions about surgical timing and alternative approaches when recovery stalls.
Why Some Patients Continue to Experience Pain After Surgery
Persistent pain after spine surgery occurs for several distinct reasons. The most common issue I encounter is that surgery addressed nerve compression but not the underlying disc pathology. Decompression procedures remove herniated material pressing on nerves. However, they don’t repair the annular tear that allowed the herniation. The damaged disc structure remains, potentially causing ongoing discogenic pain.
Adjacent segment degeneration represents another significant cause of continued symptoms. Fusion procedures eliminate motion at the treated level, increasing stress on neighboring discs. Over time, these adjacent segments may develop accelerated degeneration, herniations, or stenosis. Patients who felt better initially may develop new pain as these changes progress.
Mayo Clinic experts emphasize that patient selection and surgical timing determine outcomes more than the specific surgical technique. When surgery occurs too late, after extensive nerve damage has developed, complete recovery becomes unlikely. Chronic nerve compression causes lasting changes that decompression alone cannot reverse.
Epidural scar tissue formation can also contribute to persistent symptoms. Scar tissue may tether nerve roots or create new compression points. Muscular deconditioning from prolonged preoperative inactivity doesn’t automatically resolve after surgery. Some patients develop chronic pain patterns where the nervous system continues signaling pain even after the original structural problem is corrected. These complex scenarios require comprehensive evaluation to determine whether additional intervention might help or whether pain management strategies are more appropriate.
Looking for alternative treatments? Discover Discseel® reviews and lasting back pain relief as a non-surgical option for chronic pain after surgery.
One Lawrenceville Patient’s Experience
I’ve worked with many patients from Robbinsville and throughout the region who sought answers after back surgery didn’t deliver the relief they expected.
Dr. Wiederholz helped me tremendously with my injury after my accident. I got my facet injections with him at the surgery center and I had a great experience. The staff was very professional and caring, and Dr. Wiederholz took the time to explain everything clearly. After months of struggling with back pain following surgery elsewhere, I finally found relief through his comprehensive approach at Performance Pain and Sports Medicine.
This is one patient’s experience; individual results may vary.
Every patient’s recovery journey differs based on their specific injury, overall health, and treatment approach. When standard interventions don’t address the underlying structural problem, comprehensive evaluation at Performance Pain and Sports Medicine becomes essential to identify the true pain generator.
Conclusion
Understanding how long to recover from back surgery requires recognizing that timelines vary widely and complete healing isn’t guaranteed for everyone. While many patients experience meaningful improvement, registry data shows that roughly 65% of working patients return to work within one year of cervical spine surgery, with that number climbing to 75% by three years. The reasons for not returning to work among the remaining patients are varied and may include ongoing limitations, personal choice, or other factors. The critical factor often overlooked is that standard surgical approaches—decompression and fusion—address nerve compression but typically don’t repair the underlying annular tears and disc degeneration causing discogenic pain.
For Lawrenceville residents with persistent symptoms after surgery or those seeking alternatives before committing to fusion, emerging biologic approaches to disc repair offer mechanism-based options. The Discseel® Procedure uses fibrin sealant to seal annular tears, reduce inflammatory disc leakage, and support structural healing—targeting the root cause rather than just symptoms. A published registry study demonstrated statistically significant improvements in pain, function, and quality of life sustained over three years, with no serious adverse events reported. I evaluate each patient’s specific disc pathology through diagnostic annulargram™ to determine candidacy. If you’re experiencing persistent pain despite surgery or want to explore non-surgical alternatives, see if you may be a candidate for the Discseel® Procedure.
Need personalized help in Lawrenceville or nearby? Visit our Lawrenceville location page to learn more about advanced spine care options close to home.
This article is for educational purposes only and should not be used as a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition or treatment options. Never disregard professional medical advice or delay in seeking it because of something you have read in this article.
Frequently Asked Questions
What is the average recovery time for lumbar fusion versus microdiscectomy?
Microdiscectomy typically allows return to light activities within two to six weeks, with full recovery at three to six months. Lumbar fusion requires substantially longer—three to six months for basic function and six to twelve months for complete healing. However, these represent averages. Your individual timeline depends on age, overall health, occupation demands, preoperative symptom duration, and adherence to rehabilitation protocols. Some patients experience faster recovery while others require extended time, particularly if nerve damage occurred before surgery or if underlying disc pathology persists.
Further reading: Effective treatment options for L5-S1 disc herniation pain.
Why do some patients not fully recover after technically successful spine surgery?
Several factors contribute to incomplete recovery. Surgery often addresses nerve compression but doesn’t repair the annular tears that allowed disc herniation. The damaged disc structure remains, potentially causing ongoing discogenic pain. Adjacent segment degeneration can develop after fusion as neighboring discs experience increased stress. Epidural scar tissue may form, creating new compression points. Chronic preoperative symptoms can cause lasting nerve changes that decompression alone cannot reverse. Additionally, muscular deconditioning and psychological factors influence functional outcomes beyond the surgical repair itself. For additional insight into outcomes, visit our article on symptoms of bulging disc in neck C5-C6.
Where can I find back surgery recovery support in Lawrenceville, NJ?
Dr. Matthias Wiederholz at Performance Pain and Sports Medicine provides comprehensive evaluation and treatment for patients experiencing incomplete recovery after back surgery. Serving Lawrenceville and surrounding communities including Ewing and Hopewell, Dr. Wiederholz uses advanced diagnostic techniques to identify persistent disc pathology that may be causing ongoing pain. His quadruple board certification and expertise in regenerative medicine allow for mechanism-based treatment approaches when traditional surgery hasn’t provided complete relief. Local resources also include Capital Health Hopewell Campus and Penn Medicine Princeton Medical Center for post-surgical rehabilitation services. You can also learn about annular tear of lumbar disc and rehabilitation options.
How is the Discseel® Procedure different from traditional spine surgery?
Discseel® is a minimally invasive, non-surgical procedure that uses biologic fibrin sealant to seal annular tears, reduce disc leakage, and support structural disc healing. Unlike decompression or fusion, which address nerve compression but don’t repair disc structure, Discseel® targets the root cause—the damaged annulus fibrosus. It preserves spinal motion rather than eliminating it through fusion. Biomechanical research on fibrin-based annulus repair demonstrates that fibrin sealant can effectively seal disc defects and restore pressurization, supporting the rationale for biologic disc repair approaches. Discseel® uses diagnostic annulargram™ to identify actively leaking discs before treatment, allowing precise targeting of symptomatic levels. For more on disc repair, read about disc desiccation: causes, symptoms, and treatment.