Can A Herniated Disc Cause Spinal Stenosis? An Evidence-Based Guide by a Quadruple Board-Certified Physician
Written by Dr. Matthias Wiederholz, MD, DABA, DABPM, RMSK, FAAPMR — Board Certified in Physical Medicine & Rehabilitation, Pain Medicine, Sports Medicine, and Anti-Aging/Regenerative Medicine
Quick Insights
A A herniated disc occurs when spinal disc material ruptures and presses on nearby nerves. When this displaced tissue narrows the spinal canal, it can contribute to spinal stenosis, causing chronic nerve compression and reduced mobility. Research shows herniated discs affect up to 20 per 1,000 adults annually, with the highest risk between ages 30-50. Early medical evaluation and advanced treatments like the Discseel® Procedure offer non-surgical options for long-term relief and functional recovery.
Key Takeaways
- Herniated discs are a leading cause of degenerative spine changes, with up to 20 new cases per 1,000 adults annually.
- Disc-related spinal stenosis can cause leg pain, numbness, and, in severe cases, walking difficulty or muscle weakness.
- Not everyone with a herniated disc develops stenosis, but the risk rises with ongoing disc damage and aging.
- Regenerative, non-surgical treatments can resolve symptoms and help preserve active lifestyles, reducing the need for surgery.
Why It Matters
Understanding whether a herniated disc can cause spinal stenosis helps you take control before problems worsen. By recognizing symptoms early and considering advanced treatments, you can maintain your independence, stay active, and avoid the disruption of major spine surgery.
As a quadruple board-certified physician specializing in regenerative spine care, I know firsthand how distressing the question “can a herniated disc cause spinal stenosis?” can be for active patients in Houston, TX. Through years at Performance Pain and Sports Medicine, I have helped athletes, professionals, and parents return to their lives after sidelining back or neck injuries.
A herniated disc is when the soft, inner part of the disc—the nucleus pulposus—pushes out through the tougher outer shell, the annulus fibrosis, sometimes compressing nearby nerves. This compression can lead to a cascade of pain, nerve injury, and in some cases, the narrowing of the spinal canal itself—a process called spinal stenosis—which often threatens mobility, independence, and the ability to enjoy everyday activities.
Research demonstrates that herniated discs are responsible for up to 20 new cases per 1,000 adults yearly[1](https://www.ncbi.nlm.nih.gov/books/NBK441822/), most commonly affecting those leading active lifestyles between 30 and 50. The emotional burden—worry, frustration, and fear—is very real, especially if you’ve been sidelined by symptoms or given limited options by prior providers.
You deserve trusted answers and expert, minimally invasive solutions that prioritize long-term relief and preserve the active life you love. For more than a decade, as you can see in my doctor biography, I have remained directly involved with every patient.
What Is a Herniated Disc?
A herniated disc occurs when the soft, gel-like center (nucleus pulposus) of a spinal disc pushes through a tear in the tough outer layer (annulus fibrosis). This can press on nearby nerves, causing pain, numbness, or weakness. Most herniated discs develop in the lower back, especially between the L4-L5 and L5-S1 vertebrae. See our comprehensive guide to L5-S1 bulging discs for deeper insight.
Common Causes
The most common causes include:
- Age-related disc degeneration.
- Sudden injury or trauma.
- Repetitive strain from lifting or twisting.
In my practice, I frequently encounter patients who have spent years exploring treatments—from surgeries to pain medications—without achieving meaningful relief. Often, they are unaware that minimally invasive regenerative solutions like Discseel® can effectively restore their spine health.
Active adults are particularly at risk, often developing herniated discs after years of wear-and-tear combined with a single awkward movement. This highlights the importance of prevention and early treatment to preserve quality of life.
How Herniated Discs Affect the Spine
When disc material escapes through a tear, it can compress spinal nerves or, less commonly, the spinal cord itself. This irritation results in symptoms such as:
- Shooting pain down the legs (sciatica)
- Tingling or “pins and needles” sensations
- Muscle weakness, particularly after activity
According to research from StatPearls, herniated discs affect 1%–3% of the population, with the highest risk between ages 30 and 50.
Patients struggling with L5-S1 herniated disc symptoms or other nerve root problems may notice specific patterns that help guide effective treatment.
As a quadruple board-certified regenerative medicine specialist, I’ve observed that matching a patient’s specific spinal patterns with targeted therapies greatly increases their chances of maintaining function and avoiding escalation to more severe spinal issues.
What Is Spinal Stenosis?
Spinal stenosis is the medical term for the narrowing of the spinal canal—the space through which nerves and the spinal cord run. As this space becomes more crowded, nerves can become compressed, leading to symptoms ranging from pain and numbness to difficulty walking.
Underlying Mechanisms
Spinal stenosis can result from:
- Disc degeneration and loss of disc height.
- Thickening of ligaments around the spine.
- Bony growths (osteophytes) are forming in response to stress.
- Herniated discs pressing into the canal.
Learn more about progressive causes in our guide to lumbar degenerative disc disease.
These changes reduce the available space for nerves. Systematic reviews estimate that about 14% of older adults show signs of spinal stenosis—either by imaging or symptoms—according to recent research.
Having personally performed over 10,000 regenerative spine procedures, I’ve seen how undiagnosed stenosis can silently progress, especially in active adults who are eager to dismiss early warning signs.
Types of Spinal Stenosis
Two main forms exist:
- Central stenosis: Narrowing of the main central canal, often causing more widespread or severe symptoms.
- Foraminal stenosis: Narrowing in the small openings (foramina) where nerves exit the spine, causing pain along a specific nerve pathway.
Explore related symptoms and anatomical causes in our spinal disc tears guide.
In my clinical observation, central stenosis tends to disrupt mobility more dramatically, while foraminal stenosis may present as isolated limb pain—yet both require attentive, customized care to prevent functional decline.
The Herniated Disc-Stenosis Connection: What the Evidence
Yes, a herniated disc can directly contribute to spinal stenosis by narrowing the spinal canal and compressing nerves.
A herniated disc may:
- Protrude into the spinal canal, reducing space for nerves.
- The inflammatory response triggered by a herniated disc may cause swelling, potentially diminishing the space within the spinal canal and contributing to stenosis.
- Accelerate disc degeneration, leading to progressive instability and worsening stenosis.
In my Houston practice, it’s common to see patients whose herniated disc set off a domino effect: nerve pain first, then gradually harsher symptoms as structural problems worsen. Early, precise intervention is critical to halt this cycle.
Research shows that disc degeneration reduces the spine’s shock absorption ability and leads to instability and narrowing (stenosis) as we age.
Main Causes of Spinal Stenosis
- Degenerative disc changes
- Herniated or bulging discs
- Overgrowth of spinal ligaments or bone (osteophytes)
Learn about comprehensive treatment options for herniated disc pain.
This means disc issues are a direct and preventable pathway to spinal stenosis for many patients.
Empathetically, I reassure my patients: Just because you have a herniated disc doesn’t mean spinal stenosis is inevitable. But proactive, advanced care is your best chance to avoid that outcome—especially here in Houston, where active lifestyles are the norm.
Related Reading:
- Everything you need to know about new treatments for ruptured discs
Signs and Symptoms to Watch For
Detecting warning signs early can prevent long-term nerve damage. Common symptoms include:
- Persistent back or neck pain.
- Radiating pain down the arms or legs (sciatica).
- Numbness, tingling, or weakness in the limbs.
- Difficulty walking or balancing.
- Loss of bladder or bowel control (rare, but urgent).
In my daily practice, patients most often notice leg pain or numbness first—especially if it worsens with activity or standing. Sudden weakness or bladder changes signal a medical emergency.
When patients arrive in my Houston or Lawrenceville clinic with these warning signs, I prioritize a rapid, collaborative workup to get answers and peace of mind.
When to Seek Medical Attention
Call a board-certified spine specialist promptly if you experience:
- Sudden leg weakness.
- Bowel or bladder problems.
- Progressive, severe, or unrelenting pain.
Early intervention can mean the difference between a minor solution and prolonged disability.
For emergency guidance on disc symptoms, read about emergency symptoms of a herniated disc.
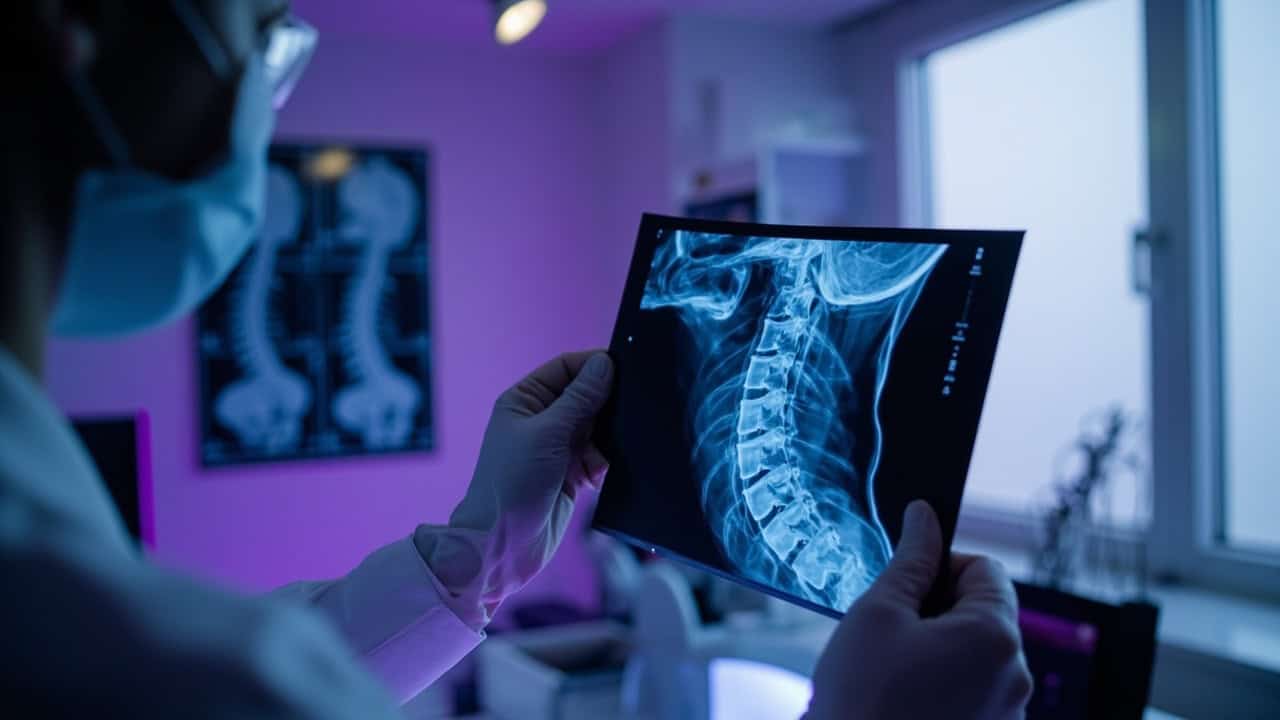
Diagnosis: How Are Herniated Discs and Spinal Stenosis Found?
Diagnosing these conditions is part art, part science. I approach each case with a combination of attentive listening, hands-on examination, and modern technology.
Physical Exam & History
I assess:
- Where and how severe your pain is
- Reflexes, muscle strength, and sensation
- Your gait and balance
A detailed neurological exam pinpoints which nerves, and at what spinal level, are involved.
Imaging and Nerve Tests
- MRI: Best for showing disc herniations, nerve root irritation, and the degree of spinal narrowing.
- CT scans: Reveal bone details, helpful if complex bone anatomy may contribute.
- Nerve conduction studies/EMG: Evaluate if and where nerve damage is occurring.
Imaging-confirmed nerve root compression, coupled with severe or persistent symptoms, is the most consistent reason to consider surgery—as highlighted in systematic reviews.
Unlike larger clinics, where you may rarely see the same provider, I personally review every MRI scan myself. This ensures nothing gets missed and that you have an advocate overseeing your entire care journey.
For more on diagnostic imaging and disc injuries, review disc desiccation and its management.
Traditional vs. Regenerative Treatment Options
Treatment should always begin with the safest, least invasive options, customized to your diagnosis and goals.
Conservative Treatments
- Physical therapy and gentle exercise.
- Nonsteroidal anti-inflammatory drugs (NSAIDs).
- Cognitive behavioral therapy (CBT).
- Activity modification and ergonomic improvements.
Clinical guidelines strongly recommend conservative treatments for both herniated discs and spinal stenosis, as documented in recent guidelines. Most patients get better over time without ever needing surgery, an outcome supported by extensive clinical evidence.
The highest recommendations among noninvasive treatments go to NSAIDs and cognitive behavioral therapy, according to a systematic review of guidelines.
Minimally Invasive and Regenerative Procedures
When pain persists or your activity is at risk, advanced interventions are available:
- Epidural steroid injections to calm inflammation.
- Advanced regenerative therapies, such as the Discseel® Procedure.
- Minimally invasive decompression.
Discseel® reviews: Achieving lasting back pain relief
As Houston’s only certified master instructor for the Discseel® Procedure, I know that properly selected regenerative options often let patients avoid surgery and return to a full life faster.
Why Choose the Discseel® Procedure?
The Discseel® Procedure is a revolutionary, minimally invasive, non-surgical treatment using a biologic fibrin sealant to repair and reinforce damaged spinal discs, stimulating your body’s own healing and collagen regeneration. For patients facing the prospect of traditional surgery or spinal fusion, Discseel® preserves mobility and offers hope for a durable solution.
Having been personally trained by Dr. Kevin Pauza—the procedure’s inventor—and as one of three master instructors worldwide, I’m able to deliver this advanced care to patients here in Houston and New Jersey, setting a national standard for minimally invasive spine treatment.
Discseel® vs Spinal Fusion
| Discseel® Procedure | Spinal Fusion | |
|---|---|---|
| Incisions/Hardware | None | Hardware, screws, and rods |
| Recovery Time | Days to weeks | Months |
| Success Rate | ~82% | Varies |
| Mobility Preservation | Yes | Motion lost at fused levels |
Cell-based and biomaterial-based therapies—like Discseel®—are emerging as especially promising therapies for disc herniation and stenosis according to recent review research. Minimally invasive decompression surgeries are another option, but still require more rigorous research before becoming the “gold standard,” as noted in expert reviews.
In my experience, Discseel® stands apart by not only sealing leaks and halting degeneration, but also helping patients reclaim life without invasive surgery. My focus is always to keep you moving, confident, and empowered—just ask the many Houston patients who’ve resumed cycling, golfing, or caring for loved ones as they did before.
Houston Patient Success Story
“Dr. Wiederholz took the time to listen, explained my options, and got me back to work quickly. I was told for years that surgery was my only choice, but after Discseel®, my pain is gone and I’m hiking again. I wish I’d found him sooner!”— Damian, Verified Google review
Experience-based insight: I personally oversee every Discseel® Procedure, which means from your first visit to your final follow-up, you’re supported by the physician with the deepest expertise—and the compassion to treat you as a whole person, not just a scan.
Meet Dr. Wiederholz — Houston’s Discseel® Authority
As a quadruple board-certified specialist and national instructor for Discseel®, I’m proud to provide Houston-area patients with world-class, personalized spine care. My boutique practice model means you’re never just a number: I combine advanced diagnostics, minimally invasive treatments, and holistic support for everything from exercise to spine-friendly daily choices. Read more about my training and experience.
I’ve performed more than 10,000 regenerative spine procedures and remain directly involved at every step of your recovery—so you feel empowered, informed, and confident you have found a true partner in your care journey.
Professional assessment: What sets my approach apart from larger centers is my commitment to seeing and hearing each patient personally, ensuring a precise diagnosis and a plan tailored to you—not a one-size-fits-all protocol.
What Our Patients Say on Google
Patient experiences are at the heart of my approach to spine care. Hearing directly from those who have faced the challenges of herniated discs and spinal stenosis helps me continually refine and personalize each treatment plan.
I recently received feedback that captures what we aim to provide for every patient seeking relief and a return to normal life. Damian, who struggled with incapacitating lumbar pain for over a year, shared his experience after undergoing the Discseel® Procedure:
“I had been in incapacitating pain and suffering from lumbar back pain for over a year due to herniated discs, Dr Wiederholz recommended the novel Discseel procedure and I can’t be happier with the results, 5 months after the procedure I’m feeling amazing and being able to return to my normal self and activities. Thank you Dr Wiederholz!” — Damian
Stories like Damian’s remind me why early, expert intervention matters—especially when it comes to preventing complications like spinal stenosis and restoring quality of life.
Herniated Disc and Spinal Stenosis Care in Houston, TX
Living in Houston, TX, means access to advanced, minimally invasive spine care that’s tailored to the needs of our diverse and active community. The city’s fast-paced lifestyle and year-round outdoor activities can put extra strain on the spine, making early recognition and treatment of herniated discs and spinal stenosis especially important.
At Performance Pain and Sports Medicine, I see firsthand how Houston’s unique blend of professionals, athletes, and families benefits from regenerative solutions like the Discseel® Procedure. Our local climate and culture encourage movement, so preserving mobility and independence is a top priority for my patients.
As Houston’s only certified master instructor for Discseel®, I’m committed to providing the highest standard of non-surgical spine care right here in our city. If you’re in Houston and concerned about back pain or spinal stenosis, I invite you to schedule a consultation and see if you’re a candidate for advanced, motion-preserving treatments.
Conclusion
The connection between herniated discs and spinal stenosis is well-established, and recognizing this relationship early is key to protecting your mobility and independence. Many of my Houston patients arrive worried about worsening pain or the threat of surgery, but with advanced regenerative care, you don’t have to accept those limits. Treatments like Discseel® and other minimally invasive options can relieve pain, restore function, and help you return to the activities you love—without major surgery or long recovery.
As a quadruple board-certified physician and master instructor for Discseel®, I am dedicated to providing personalized, compassionate care that addresses both the physical and emotional impact of spinal conditions. Advanced regenerative care, without invasive surgery, is not just a promise—it’s my daily practice. If you’re ready to stop missing out on life due to back pain, I invite you to see if you are a candidate for the Discseel® Procedure and take the first step toward lasting relief in Houston, TX.
This article is for educational purposes only and should not be used as a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition or treatment options. Never disregard professional medical advice or delay in seeking it because of something you have read in this article.
Frequently Asked Questions
Can a herniated disc cause spinal stenosis?
Yes, a herniated disc can contribute to spinal stenosis by narrowing the spinal canal and compressing nerves. This process may lead to pain, numbness, or weakness in the legs. Not everyone with a herniated disc develops stenosis, but the risk increases with ongoing disc damage and aging. For more details, see herniated disc symptoms, causes, and treatment.
Where can I find non-surgical spine care for herniated discs and spinal stenosis in Houston, TX?
You can find advanced, non-surgical spine care—including the Discseel® Procedure—at my Houston practice, Performance Pain and Sports Medicine. I offer prompt appointments, thorough evaluations, and personalized regenerative treatments designed to help you regain mobility and avoid unnecessary surgery.
What is the success rate of regenerative treatments like Discseel® for spinal stenosis?
Regenerative treatments such as Discseel® have shown an 82% success rate in relieving pain and preserving spinal mobility, which is significantly higher than traditional spinal fusion. Most patients experience meaningful improvement and a rapid return to daily activities, often within days of the procedure.
Ready to regain your active lifestyle? Contact us today and discover your options for lasting relief.