By Dr. Matthias Wiederholz with Performance Pain and Sports Medicine
Quadruple Board-Certified in Physical Medicine & Rehabilitation, Pain Medicine, Sports Medicine, and Anti-Aging & Regenerative Medicine
Updated January 29, 2026
Medically reviewed and updated for accuracy
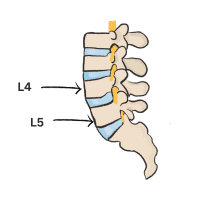
Understanding L4-L5 Nerve Root Compression Symptoms
The L4-L5 spinal segment—located between the fourth and fifth lumbar vertebrae—is one of the most common sites of disc-related problems in the lower back. When disc herniation, bulging, or degeneration occurs at this level, the resulting nerve compression can produce a distinct pattern of symptoms that significantly impact daily function.
Patients experiencing L4-L5 nerve root compression symptoms often describe radiating leg pain, numbness, tingling, and weakness that follows specific pathways depending on which nerve root is affected. Understanding these symptom patterns is essential for accurate diagnosis and effective treatment planning.
Quick Insights: L4-L5 Nerve Root Compression Symptoms
- L4-L5 is the most commonly affected lumbar segment for disc herniation and nerve compression
- L4 nerve root symptoms differ from L5 nerve root symptoms in their distribution patterns
- Early recognition and treatment can prevent progression to chronic pain and functional disability
- Conservative care remains effective for many patients, with advanced interventional options available when needed
L4 Versus L5 Nerve Root Symptoms: Understanding the Differences
One of the most important distinctions in diagnosing L4-L5 pathology is differentiating between L4 and L5 nerve root compression. While both originate from the same spinal segment, they produce different symptom patterns based on their anatomical pathways.
L4 Nerve Root Compression Symptoms
When the L4 nerve root is compressed—typically by a disc herniation at the L3-L4 or L4-L5 level—patients experience:
- Pain distribution: Lower back pain radiating down the front and inner thigh to the inner knee and shin
- Numbness and tingling: Inner thigh, knee, and medial lower leg
- Weakness: Difficulty extending the knee (straightening the leg); weak quadriceps muscle
- Reflex changes: Diminished or absent patellar (knee-jerk) reflex
- Functional impact: Trouble climbing stairs, rising from a seated position, or standing on tiptoes
Research demonstrates that patient-reported pain patterns may not always follow classic dermatomal distributions, which underscores the importance of combining clinical examination with imaging studies for accurate diagnosis.
L5 Nerve Root Compression Symptoms
L5 nerve root compression—most commonly from L4-L5 disc herniation—produces a different symptom pattern:
- Pain distribution: Lower back pain radiating down the lateral thigh, lateral leg, and top of the foot to the big toe
- Numbness and tingling: Lateral calf, top of foot, and webspace between first and second toes
- Weakness: Difficulty with foot dorsiflexion (lifting the foot upward); weak anterior tibialis and extensor hallucis longus muscles
- Functional impact: Foot drop when walking, difficulty walking on heels, tripping hazard
- Reflex changes: Typically normal patellar and Achilles reflexes (though medial hamstring reflex may be affected)
L5 radiculopathy is statistically the most common lumbar nerve root compression, accounting for a significant proportion of sciatica cases related to L4-L5 disc pathology.
Comprehensive L4-L5 Pain Symptoms and Patterns
Beyond nerve-specific symptoms, L4-L5 pathology produces a range of pain patterns that can vary in intensity, duration, and character depending on the underlying cause.
Axial Lower Back Pain
Many patients with L4-L5 disc problems experience localized lower back pain even without significant nerve compression. This axial pain typically results from:
- Disc degeneration: Loss of disc height and hydration causing mechanical instability
- Annular tears: Tears in the outer disc wall that can leak inflammatory proteins and cause chemical irritation
- Facet joint arthritis: Wear and tear of the small joints in the back of the spine
- Muscular strain: Compensatory muscle tension and spasm protecting the injured segment
This localized pain often worsens with forward bending, prolonged sitting, lifting, or twisting movements. Patients may experience stiffness after periods of inactivity, particularly in the morning.
Radicular Pain (Sciatica)
When L4-L5 disc material compresses a nerve root, the resulting radicular pain—commonly called sciatica—can be severe and disabling. Research comparing surgical and nonsurgical management of lumbar radiculopathy shows that leg pain often responds differently than back pain, with some patients experiencing significant leg pain relief while back pain persists.
Radicular pain characteristics include:
- Sharp, shooting quality: Often described as electric, burning, or stabbing
- Follows nerve pathway: Travels from the lower back down the leg in the distribution described above
- Worsens with certain positions: Sitting, forward bending, coughing, or sneezing may increase symptoms
- Relief with specific positions: Many patients find relief standing, walking, or lying with legs elevated
Referred Pain to Hip and Buttock
A common question patients ask is whether L4-L5 problems can cause hip pain. The answer is yes—L4-L5 pathology frequently produces pain in the hip and buttock regions through several mechanisms:
- Nerve irritation: The L4 and L5 nerve roots contribute to the sciatic nerve, which passes through the buttock region
- Muscle compensation: Patients often alter their gait and posture to protect the painful spine, leading to hip muscle strain
- Referred pain patterns: The brain can mislocalize pain signals from the lower back to the hip and buttock
- Facet joint referral: L4-L5 facet joint arthritis commonly refers pain to the hip and groin
Clinical evaluation is essential to distinguish true hip joint pathology from referred pain originating at the L4-L5 segment, as treatment approaches differ significantly.

What Causes L4-L5 Nerve Root Compression?
Understanding the underlying causes of L4-L5 nerve compression helps patients and physicians develop targeted treatment strategies.
Disc Herniation and Bulging
Disc herniation at L4-L5 is the most common cause of nerve root compression at this level. Clinical trials comparing discectomy with conservative care demonstrate that disc herniation severity and duration significantly impact treatment outcomes. When the gel-like nucleus pulposus pushes through a tear in the annulus fibrosus, it can directly compress the adjacent nerve root.
Disc bulging—a less severe form where the disc protrudes without frank herniation—can also produce symptoms, particularly when the spinal canal is already narrow from other factors.
Annular Tears and Disc Degeneration
Foundational anatomic research on annular tears in the lumbar spine has established that tears in the disc’s outer wall are both common and clinically significant. These tears can occur from:
- Repetitive loading and mechanical stress
- Age-related disc degeneration
- Traumatic injury (lifting, falls, motor vehicle accidents)
- Poor posture and body mechanics
Longitudinal imaging studies have demonstrated a strong correlation between annular tears and progressive disc degeneration. These tears not only weaken the disc structure but can also leak inflammatory chemicals that irritate nearby nerve roots, contributing to both local and radiating pain.
Spinal Stenosis at L4-L5
Spinal stenosis—narrowing of the spinal canal—frequently occurs at L4-L5 due to age-related changes including:
- Thickening of the ligamentum flavum (the ligament lining the back of the spinal canal)
- Facet joint hypertrophy and bone spur formation
- Disc bulging reducing the available space for nerves
- Loss of disc height causing the vertebrae to settle closer together
When stenosis develops at L4-L5, patients often experience worsening symptoms with prolonged standing or walking (neurogenic claudication) and relief when sitting or bending forward.
Spondylolisthesis
Spondylolisthesis—when one vertebra slips forward relative to the one below—commonly occurs at L4-L5 due to this segment’s mobility and weight-bearing stress. This slippage can narrow the neural foramina (the openings through which nerve roots exit the spine), causing compression of the L4 or L5 nerve roots.
Diagnostic Approaches for L4-L5 Pathology
Accurate diagnosis of L4-L5 nerve root compression requires a comprehensive evaluation combining clinical examination with advanced imaging.
Clinical Examination
During evaluation, I perform specific tests to identify which nerve root is affected:
- Straight leg raise test: Reproduces radicular pain by stretching the sciatic nerve
- Motor strength testing: Assesses quadriceps (L4) and anterior tibialis (L5) strength
- Sensory examination: Maps areas of numbness or altered sensation
- Reflex testing: Evaluates patellar and Achilles reflexes
- Gait analysis: Observes for foot drop or antalgic gait patterns
Imaging Studies
MRI remains the gold standard for visualizing disc pathology, nerve compression, and soft tissue changes at L4-L5. CT scans may be used when MRI is contraindicated, particularly to evaluate bony structures. Plain X-rays help assess alignment, disc space height, and the presence of spondylolisthesis.
Advanced diagnostic techniques like diagnostic selective nerve root blocks can help confirm which specific nerve root is generating symptoms when imaging findings are unclear or multiple levels show abnormalities.
Conservative and Interventional Treatment Approaches
Research on the efficacy of conservative treatment for lumbar disc herniation demonstrates that many patients achieve substantial improvement with nonoperative care over a two-year period. However, the optimal approach depends on symptom severity, functional impairment, and individual patient factors.
Conservative Management
Initial conservative treatment for L4-L5 nerve root compression typically includes:
- Activity modification: Avoiding aggravating positions while maintaining mobility
- Physical therapy: Core strengthening, nerve gliding exercises, and postural training
- Anti-inflammatory medications: NSAIDs to reduce inflammation around compressed nerves
- Neuropathic pain medications: For managing nerve-related pain when appropriate
- Epidural steroid injections: Targeted delivery of anti-inflammatory medication to the affected nerve root
Many patients respond well to this staged approach, with systematic reviews showing that conservative care can yield outcomes comparable to surgery in appropriately selected patients, particularly when symptoms have been present for less than six weeks.
When Conservative Care Is Insufficient
Some patients continue to experience significant pain and functional limitation despite comprehensive conservative management. Research comparing discectomy with standardized nonoperative care shows that surgical intervention can provide superior leg pain relief in chronic disc herniation, with benefits particularly evident at the L4-L5 level.
Indications that more advanced intervention may be warranted include:
- Progressive neurological deficit (worsening weakness or numbness)
- Severe pain unresponsive to conservative measures for 6-12 weeks
- Cauda equina syndrome (medical emergency requiring urgent surgery)
- Significant functional impairment affecting work or quality of life
The Discseel® Procedure: A Regenerative Approach to L4-L5 Disc Pathology
For patients whose L4-L5 pain stems from annular tears and disc degeneration rather than large herniated fragments, the Discseel® Procedure offers a biologic alternative to traditional surgery. This innovative treatment addresses the underlying disc pathology by sealing tears in the annulus fibrosus and promoting natural healing.
How Discseel® Addresses L4-L5 Disc Pathology
The Discseel® Procedure utilizes an FDA-approved fibrin biologic sealant to repair damaged discs at the L4-L5 level. Unlike surgical approaches that remove disc material or fuse vertebrae, this minimally invasive treatment works with the body’s natural healing mechanisms:
- Precise tear identification: Advanced imaging (Annulogram™) identifies the exact location and extent of annular tears
- Biologic sealing: Fibrin sealant is delivered directly into the disc to seal tears and prevent further leakage of inflammatory material
- Natural healing: The fibrin creates a scaffold for the body’s own repair cells to regenerate disc tissue
- Preserved motion: Unlike fusion, Discseel® maintains natural spinal mobility at L4-L5
Clinical research published in peer-reviewed literature demonstrates that intradiscal fibrin sealant appears safe and may improve both pain and function in patients with symptomatic lumbar disc disruption, including at the L4-L5 level.
The Discseel® Procedure Process
The procedure follows a carefully orchestrated sequence:
- Comprehensive Evaluation: Detailed consultation, review of imaging, and discussion of treatment goals
- Annulogram™ Testing: Advanced diagnostic imaging that replaces traditional discography, precisely mapping annular tears
- Treatment Day: Minimally invasive injection of fibrin biologic under imaging guidance
- Recovery Period: Gradual return to activity as the fibrin promotes disc healing over several months
Most patients return to light activities within days and progressively increase activity levels as healing occurs. The fibrin continues to facilitate tissue regeneration for up to a year following treatment.
Who May Benefit from Discseel® for L4-L5 Pathology
Ideal candidates for the Discseel® Procedure include patients with:
- Confirmed annular tears at L4-L5 on imaging
- Discogenic pain (pain originating from the disc itself)
- Radicular symptoms related to disc inflammation rather than large herniated fragments
- Unsatisfactory response to conservative care but desire to avoid surgery
- Multiple-level disc problems where fusion would sacrifice too much mobility
As the first physician trained in the Discseel® Procedure in Houston and New Jersey, I carefully evaluate each patient to determine if this innovative treatment is appropriate for their specific L4-L5 pathology.
Learn more about patient experiences and outcomes with the Discseel® Video Resource Center, where you can watch detailed explanations of the procedure and hear from patients who have undergone treatment.
Real Patient Testimonial
Watch this patient share their experience with the Discseel® Procedure:

Clinical Evidence Supporting L4-L5 Treatment Approaches
The management of L4-L5 nerve root compression and disc pathology is supported by substantial clinical research. A multicenter pilot study published in Pain Physician examined the use of intradiscal fibrin sealant in adults with chronic discogenic low back pain, including patients with L4-L5 pathology.
The study findings demonstrated:
- No significant adverse changes in neurological assessments, X-ray, or MRI findings
- Decreased mean low back pain scores over 26, 52, and 104 weeks
- Improved disability scores (Roland-Morris Disability Questionnaire)
- Safety profile appropriate for outpatient interventional spine care
These results align with the clinical outcomes we observe in practice when treating L4-L5 disc pathology with biologic approaches. The key is appropriate patient selection and understanding which disc pathology patterns respond best to regenerative versus surgical interventions.
Related Conditions and Considerations
L4-L5 pathology often occurs in the context of broader lumbar spine problems. Understanding these related conditions helps patients and physicians develop comprehensive treatment strategies.
Multi-Level Disc Disease
Many patients have disc problems at adjacent levels—for instance, both L5-S1 and L4-L5. The presence of multi-level disease may influence treatment planning, as addressing all symptomatic levels is important for optimal outcomes.
General Disc Pathology Considerations
The principles that apply to herniated disc symptoms and treatment generally extend to L4-L5 specifically, though the nerve root affected determines the specific symptom pattern.
Frequently Asked Questions About L4-L5 Nerve Root Compression
What are the most common symptoms of L4-L5 nerve compression?
The most common symptoms include radiating leg pain following either the L4 or L5 nerve distribution, numbness or tingling in specific areas of the leg and foot, weakness in the leg muscles (particularly difficulty lifting the foot or extending the knee), and lower back pain that worsens with sitting, bending, or lifting. The exact symptom pattern depends on whether the L4 or L5 nerve root is primarily affected.
How do I know if I have L4 versus L5 nerve root compression?
L4 nerve compression typically causes pain down the front of the thigh to the inner knee and shin, weakness when straightening the knee, and numbness on the inner thigh and shin. L5 nerve compression causes pain down the outer thigh and leg to the top of the foot, weakness lifting the foot upward (foot drop), and numbness on the outer calf and top of the foot between the first and second toes. A thorough clinical examination combined with MRI imaging provides definitive diagnosis.
Can L4-L5 problems cause hip and buttock pain?
Yes, L4-L5 disc pathology frequently produces pain in the hip and buttock regions through multiple mechanisms. Nerve irritation from L4-L5 disc herniation commonly refers pain to these areas. Additionally, the L4 and L5 nerve roots contribute to the sciatic nerve, which passes through the buttock. Facet joint arthritis at L4-L5 also commonly refers pain to the hip and groin. Compensatory muscle strain from altered posture and gait further contributes to hip region discomfort.
What is L4-L5 spinal stenosis and how does it differ from disc herniation?
L4-L5 spinal stenosis is narrowing of the spinal canal at this level, often from age-related changes including thickened ligaments, bone spurs from arthritis, and bulging discs. Unlike acute disc herniation, which typically causes sudden onset of symptoms, stenosis develops gradually. Stenosis often causes neurogenic claudication—leg pain and weakness that worsens with standing or walking and improves with sitting or bending forward. Some patients have both stenosis and disc herniation simultaneously, requiring careful diagnostic evaluation.
How long does it take for L4-L5 nerve compression to heal?
Recovery timelines vary significantly based on the underlying cause and severity of compression. Research shows that many patients with disc herniation experience significant improvement within 6-12 weeks of conservative care. However, some patients continue to have symptoms beyond this timeframe. Early leg pain relief often occurs before complete resolution of back pain. When conservative care is insufficient, interventional treatments like epidural injections or procedures like Discseel® can accelerate healing. Persistent symptoms beyond 12 weeks despite appropriate conservative care warrant consideration of advanced interventions.
When should I consider surgery versus minimally invasive treatments for L4-L5 problems?
Surgery is typically considered for progressive neurological deficit (increasing weakness or numbness), cauda equina syndrome (a medical emergency), or severe pain unresponsive to comprehensive conservative care for 6-12 weeks. Minimally invasive treatments like the Discseel® Procedure may be appropriate for patients with confirmed annular tears and discogenic pain who desire to avoid surgery while addressing the underlying disc pathology. The decision depends on your specific diagnosis, symptom severity, functional goals, and response to initial treatments. A thorough evaluation helps determine the most appropriate treatment pathway.
Taking the Next Step: Expert Care for L4-L5 Nerve Root Compression in Houston
If you’re experiencing L4-L5 nerve root compression symptoms—whether radiating leg pain, numbness, weakness, or persistent lower back pain—expert evaluation is the first step toward effective treatment and recovery.
At Performance Pain and Sports Medicine, we offer comprehensive diagnostic evaluation and a full spectrum of treatment options, from conservative care to advanced interventional procedures like the Discseel® Procedure. Our approach is tailored to your specific pathology, symptom severity, and treatment goals.
I’m available for consultations at our Houston location, where we provide state-of-the-art care for complex spinal conditions. As the first physician trained in the Discseel® Procedure in Houston, I bring extensive experience in both traditional and innovative approaches to managing L4-L5 pathology.
Don’t let L4-L5 nerve compression control your life. Contact us today to schedule a consultation, or complete our Discseel® candidacy form to learn if this innovative treatment may be right for you.
Medical Disclaimer
This article is for educational purposes only and does not constitute medical advice. Every patient’s condition is unique, and treatment recommendations must be individualized based on comprehensive evaluation by a qualified physician. The information presented here does not guarantee specific outcomes and should not be used as a substitute for professional medical consultation. Always consult with a board-certified pain management physician or spine specialist before making decisions about your care.